Dear colleagues, I share this case with you despite the fact that success or failure has yet to be definitively shown as I think it throws up some interesting points or questions to consider. I hope you enjoy it! Best wishes, Simon Barnwell
Presenting complaint
Pain on biting and touching front tooth
Key clinical findings
- UL1 only tooth to be TTP
- UL1 Buccal palpation tenderness
- UL1 unresponsive to cold test
- UR1 and UL2 responsive to cold test
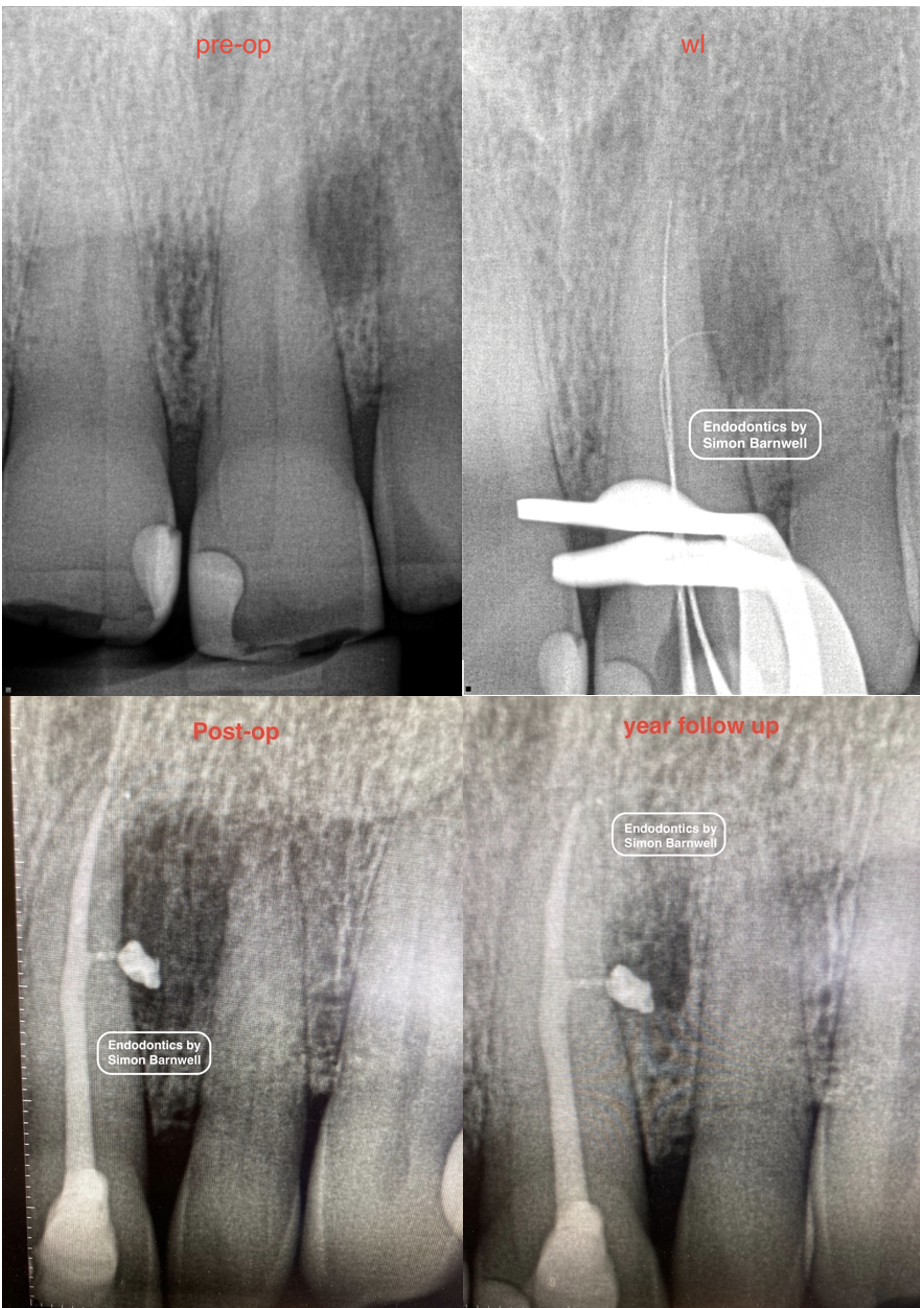
Key radiographic findings
- Visible root canal space UL1
- Deep composite restoration UL1
- Large lateral peri-radicular radiolucency
- The pre-op radiograph was taken using a new sensor holder which have left some unusual artifacts on the pre-op radiograph (look at the horizontal and vertical lines seen on the clinical crowns of UR1 and UL1). That new holder was not used again!
Diagnosis
Symptomatic apical periodontitis UL1
Key features of treatment
- Necrotic pulp found on access
- 3% sodium hypochlorite main irrigant
- Main canal shaping completed up to a WaveOne® Gold medium
- Scouting for a lateral canal with pre-curved size 8 k file
- Working length radiograph taken instead of cone fit radiograph due to suspicion that a file had been inserted successfully into the lateral canal
- Lateral canal explored and prepared with pre-curved k files size 8,10,15,20
- Inter-appointment calcium hydroxide paste placed with a lentulo spiral filler into dried canal
- Symptom resolution on return for second visit
- Irrisafe® tip used for PUI for 17% EDTA and for sodium hypochlorite
- Obturation with warm vertical compaction technique and TotalFill® BC Sealer HiFlow™
- Lateral canal sealed, with large sealer puff seen
- 1 year follow up delayed due to Covid 19
- The tooth is symptom free and the lesion seems smaller but has not healed at 2 year follow up
- Patient consent to share information about the case
Points for discussion
- It is interesting to see such a large apical lesion, which potentially leads to additional caution being required during the diagnostic process
- It is interesting to see an instrumentable lateral canal
- Inconsistencies are seen in the appearance of the radiographs, making evaluating change in the size of the lateral lesion over time harder to evaluate
- A large bioceramic sealer puff is present laterally and this appears to show no sign of resorption/ dissolution 2 years post-treatment. Are concerns relating to bioceramic sealer solubility
- Will this go on to heal with more time? Or will I need to consider a surgical approach in due course?
- This lateral lesion is healing slowly. Has attempting to clean and seal this lateral canal actually improved the situation? Is it better to clean it as it has been cleaned here and accept the (inevitable?) sealer puff that follows? Or would ignoring the lateral canal and perhaps not getting such a lateral canal clear fill and lateral canal sealer puff have been a better option?












